Introduction
Welcome back to the second part in our Restrictive Surgery series! Last week we covered adjustable gastric bands and I hope you’ve adjusted (get it?) to following our flow here at this blog because its all about distributing proper information to all, while maintaining a bit of sanity with some humor (humour for our british readers, if there are any).

Let’s get this started then, today its all about Laparoscopic Sleeve Gastrectomy (LSG). First let me break down these words for you:
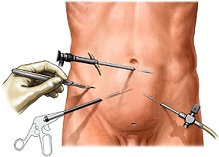
Laparoscopy refers to using small incisions so different “ports” can be installed in the skin to access a cavity, in this case the abdomen, with different tools that grasp tissue, cut, suture, etc.
Sleeve refers to the shape of the stomach that remains after the removal of part of the stomach. Gastrectomy comes from the greek roots gaster (stomach) and ektome (removal of); so this gives us “removing the stomach”. But in reality only a portion of the stomach is removed (see picture below).

If we put all three words together we get a procedure that consists of removing a part of the stomach, leaving behind a “sleeve” shaped stomach, all while being done laparoscopically (aka minimally invasive).
Now that we know what a LSG is, the question we have to ask ourselves is: Why?
The answer, I fear, is not so simple. But that’s why you have me, to walk you through this!
When we talked last week about restrictive procedures we mentioned that these act by forcing the patient to eat less. If a person has a smaller stomach, how can he/she eat more right? In the case of the AGB this was the only mechanism that was at play. But there’s something special about LSG, let’s dive deeper into this subject (or as they say in Inception “We must go deeper”).
How is LSG performed?
- The surgeon makes very small incisions on the abdomen (amount of incisions varies by technique, surgeon or equipment), where ports are placed so that a camera and many other surgical tools can pass through.
- The stomach is inflated through an apparatus called a bougie (think of this as an inflatable tube) so that the surgeon can determine the size and shape of the stomach sleeve that will remain after excising the fundus, part of the body and antrum.
- After excising the aforementioned parts, the sleeve is stapled shut, the ports are removed from the abdomen and the small incisions are sutured shut.
What’s so different about Sleeve Gastrectomy?
Sleeve gastrectomy involves removing part of the stomach, this is what puts it in the restrictive category of bariatric procedures. But here’s where things get weird: the part of the stomach that’s left isn’t the only main act in this show, its co-star is actually the part that’s removed!
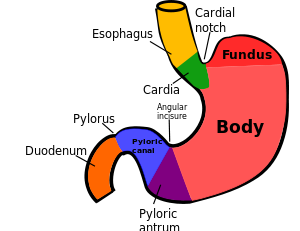
The stomach is an important part of the gastrointestinal tract, it has various functions; it secretes hydrochloric acid so different molecules in food can be broken down, its muscle fibers contract to “churn” food and turn it into what is called chyme (partially digested food) and it plays an important role in the regulation of huger by the brain via signaling with a hormone called Ghrelin.
This hormone is produced by P/D1 cells located in the fundus of the stomach. Since most of the fundus is removed during LSG, there will be far less ghrelin telling your brain that you should feel hungry.
Please take note that we WILL do a concise review on how hunger/satiety is regulated in the brain in a future blog post!
Now that we have all the pieces of this puzzle lets do a quick recap
- Sleeve gastrectomy reduces the size of the stomach
- It takes less food to feel satisfied
- Less food means diminished caloric intake
- Diminished caloric intake means the body uses its energy stores (fat)
- The body uses its energy stores, patient loses weight
- Sleeve gastrectomy greatly reduces the amount of ghrelin
- Less ghrelin means less hunger
- Less hunger means less food intake
Conclusion
We can correctly deduce that LSG employs a two-way approach at treating obesity: forcing the patient to eat less because of its restrictive aspect and helping the patient battle cravings and unhealthy eating habits by curbing appetite.
This extra boost in curbing appetite really has set LSG apart from other bariatric procedures. Additionally, the knowledge that ghrelin stimulates appetite is relatively new (1) and its importance is just being further strengthened by the latest research (2, 3).
The above mentioned statements plus the fact that it is a simple procedure coupled with great weight loss and low side effects, have made Sleeve Gastrectomy bariatric surgery’s rising star. With more and more research showing up that supports LSG as a primary procedure, its time for gastric bypass to watch its back, there’s a new kid in town!!!
Next week we will continue with the next type of bariatric procedures: the malabsorptive category.
But for now relax, sit back and enjoy life!
Have a great week!
-LIMARP Blog
References
1) Tschöp M, Smiley DL, Heiman ML. Ghrelin induces adiposity in rodents. Nature. 2000;407(6806):908–13.
2) Bohdjalian A, Langer FB, Shakeri-Leidenmühler S, Gfrerer L, Ludvik B, Zacherl J, et al. Sleeve gastrectomy as sole and definitive bariatric procedure: 5-year results for weight loss and ghrelin. Obesity surgery. 2010;20(5):535–40.
3) Wang Y, Liu J. Plasma Ghrelin Modulation in Gastric Band Operation and Sleeve Gastrectomy. Obes Surg. 2009;19:357–62.



