Women’s health, along with their rights to proper care and ownership of their bodies, has come a long way in the last few decades, this is due to the political movements that made this progress happen and to the emerging medical and clinical research that has finally focused on women as their sole study cases.
This new research has shown a new light on how different illnesses or conditions affect women differently than men, such as obesity, depression, cancer, and reproductive issues.
It has also helped the medical world, and us by extension, learn more about disorders that only affect women, as is the case with polycystic ovary syndrome. This syndrome is more common than one may think and most of the time it goes by undiagnosed, so for this article, we will talk more about polycystic ovary syndrome, as well as its causes, symptoms, and the best ways to lose weight while having PCOS.
At LIMARP®, we care about our patient’s health and we strive to provide the best medical attention possible. Our team, led by Dr. Liza María Pompa González, is highly qualified to provide the information and treatment you need, as well as to guide you and answer any questions that may arise during and after your initial consultation. Our team also has expert nutritionists that can provide a diet plan that will best serve your needs if you’ve been diagnosed with PCOS.
As always, we’d like to remind you that the information we’re about to present about polycystic ovary syndrome is general and illustrative, so it may not apply to every case; this is why it’s important to contact your doctor if you start seeing any irregularities in your period or if you’re experiencing any uncomfortable symptoms. If the diet provided to you doesn’t work or if you’re gaining weight instead of losing it, contact your doctor right away so that they can work on finding a solution.
What is polycystic ovary syndrome (PCOS)?
Before diving into causes and symptoms, as well as the best way to lose weight, it’s important to clear up any doubts regarding polycystic ovary syndrome (PCOS, for short). This means explaining what it is and who can get it, as well as a bit of history when it was described. We believe it’s important for women to be aware of the medical conditions that can affect them, and although they may never experience them, someone close to them might.
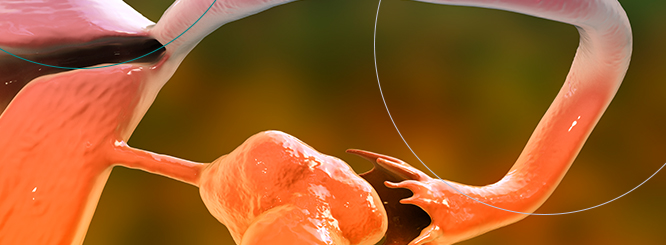
To start with a little bit of medical history, PCOS was first described as an endocrine disorder in 1935 by American gynecologists Irving F. Stein Sr. and Michael L. Leventhal, and it has now become recognized as one of the most common causes of oligo ovulatory infertility among women[1]. Ever since then, PCOS has been thoroughly researched and it’s now known as a health problem caused by an imbalance of reproductive hormones. The name polycystic comes from the characteristic cysts that form on the ovaries, which are some of the main signs that a woman has developed PCOS.
This hormone imbalance can also affect the ovaries in the sense that they may not develop healthy eggs or if they do, they’re not released during ovulation[2]. Aside from the cysts, PCOS can cause missed or irregular periods, which can later lead to infertility.
Who can get polycystic ovary syndrome (PCOS)?
Between 5% and 10% of women between 15 and 44, or childbearing years, have PCOS, and they’re more commonly diagnosed when they’re in their 20’s or 30’s[3].
However, your risk of developing PCOS increases if you have obesity or if this syndrome is common in your family.
The percentage of women who can get PCOS is also very high with one study[4] stating that up to 26.7% percent of women in the aforementioned age group have this syndrome, but despite these numbers, PCOS still goes widely undiagnosed or it takes several doctor visits, sometimes with different one, to get a proper diagnosis. This delay can cause frustration for patients and it can lead to development of other serious comorbidities if their PCOS is not treated properly.
Polycystic ovary syndrome has three features[5] and if you present two of the following ones, you can be diagnosed with PCOS:
- Irregular periods
- Excess androgen
- Polycystic ovaries
However, we recommend that you get a clear diagnosis from your doctor before starting any treatment that involves medication or any other type of medical intervention.
Causes for polycystic ovary syndrome (PCOS)
Doctors and researchers still haven’t found a clear cause for PCOS, but there are several factors that can increase a woman’s chance of developing polycystic ovary syndrome. The first one, as we have previously mentioned, is due to genetics, although the specific genes associated with the condition have not yet been identified[6].
Another probable cause for polycystic ovary syndrome is insulin resistance. Insulin is produced naturally by the pancreas to control the amount of sugar in our blood, but when a person has insulin resistance, their body’s tissues become resistant to the effects of insulin; thus, the body begins to produce more in order to compensate for the apparent lack.
The high levels of insulin causes the ovaries to produce too much testosterone, preventing the development of follicles and healthy ovulation.
It can also lead to weight gain, which in turn makes the body produce more insulin, worsening the symptoms of PCOS and putting women at risk of developing type 2 diabetes. Studies[7] have shown that 70% of women with PCOS also have insulin resistance.
Hormone imbalance can also lead to PCOS and the women who have been diagnosed with this syndrome tend to lack or overproduce the following hormones:
- Raised levels of testosterone.
- High levels of luteinising hormone, which stimulates ovulation, but can affect the ovaries if the level rises.
- Low levels of sex hormone-binding globulin.
- High levels of prolactin, which can affect the breast glands that produce milk.
Polycystic ovary syndrome symptoms
Like with almost every other condition, symptoms for PCOS may vary from woman to woman; this means that some may not present symptoms or only mild ones, while others may suffer from intense or severe ones. Many women start noticing symptoms around their teenage years or in their early 20’s and these are some of them:
- Irregular periods
- Excessive hair growth (hirsutism)
- Acne
- Weight gain
- Hair loss
- Difficulty getting pregnant
Having PCOS doesn’t mean you can’t get pregnant at all and there are treatment options that can help you ovulate. Talk with your doctor if you’re trying to get pregnant and/or if you present any of the aforementioned symptoms.
How to Lose Weight with PCOS
There are many reasons why people with PCOS find it difficult to lose weight, such as hormonal imbalances, insulin resistance, and inflammation. It’s important to stay motivated throughout the weight loss journey, especially since one study[8] reported that even a small weight loss of about 5% can improve insulin resistance, hormone levels, menstrual cycles, fertility, and overall quality of life in people with PCOS.
Many women have tried to lose weight but have failed to do so by following crash diets or types of physical activities that don’t benefit them. We strongly recommend our patients to learn more about the type of food they eat, as well as to understand how PCOS alters their bodies, in order to successfully lose weight. Next, we’ll present some ways that women with PCOS can lose weight, as well as a brief explanation on how supplements can make this process easier.
As part of your new diet plan to lose weight, your nutritionist will recommend that you reduce your carb intake to reduce your insulin levels. In one study[9], people with PCOS followed a three week diet that consisted of 40% carbs and 45% fat and then another three week diet of 60% carbs and 25% fat. Protein intake was 15% of total daily calories during each phase. While blood sugar levels were similar during the two phases of the diet, insulin levels went down 30% during the lower carb, higher fat phase.
There are other changes that can be done to your diet if you have PCOS and want to lose weight, such as:
- Increasing fiber intake: In one study[10], higher fiber intake was linked to lower insulin resistance, less total body fat, and less belly fat in people with PCOS.
- Adding fermented foods: Eating foods high in probiotics may help increase the number of beneficial bacteria in your gut, thus, stimulating your metabolism and being able to lose weight.
- Limiting processed foods and added sugars: People with PCOS may process sugar differently than those without it, as research[11] shows that women with PCOS experience larger spikes in blood sugar and insulin levels after consuming the same amount of sugar as women without this condition.
Supplements to Manage PCOS
Taking supplements while having PCOS can also help you to lose weight. Many studies have shown that the following supplements can help people, not only by reducing their insulin levels, but by actually allowing them to lose weight.
Some of the supplements that have been researched include myo-inositol, inositol, and carnitine.
Of course, we highly recommend that you talk to your doctor before taking any of these supplements to ensure that you lose weight in an effective and healthy way.
Contact Us to Learn More
If you want to learn more about the best way to lose weight while having PCOS, schedule an appointment with one of our doctors. We can help determine the right treatment for you. Contact us online anytime or give us a call at (619) 373-0229.
References
- [1] Barry JA, Azizia MM, Hardiman PJ. Risk of endometrial, ovarian and breast cancer in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2014 Sep-Oct;20(5):748-58. doi: 10.1093/humupd/dmu012. Epub 2014 Mar 30. PMID: 24688118; PMCID: PMC4326303.
- [2] “Polycystic ovary syndrome”. https://www.womenshealth.gov/a-z-topics/polycystic-ovary-syndrome. (Accessed June 25, 2023).
- [3] Trivax, B., & Azziz, R. (2007). Diagnosis of polycystic ovary syndrome. Clinical Obstetrics and Gynecology, 50(1), 168–177.
- [4] March WA, Moore VM, Willson KJ, Phillips DI, Norman RJ, Davies MJ. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Hum Reprod. 2010 Feb;25(2):544-51. doi: 10.1093/humrep/dep399. Epub 2009 Nov 12. PMID: 19910321.
- [5] “Polycystic ovary syndrome”. https://www.nhs.uk/conditions/polycystic-ovary-syndrome-PCOS/. (Accessed June 25, 2023).
- [6] Goyal A, Ganie MA. Idiopathic Hyperprolactinemia Presenting as Polycystic Ovary Syndrome in Identical Twin Sisters: A Case Report and Literature Review. Cureus. 2018 Jul 19;10(7):e3004. doi: 10.7759/cureus.3004. PMID: 30250766; PMCID: PMC6145756.
- [7] Marshall JC, Dunaif A. Should all women with PCOS be treated for insulin resistance? Fertil Steril. 2012 Jan;97(1):18-22. doi: 10.1016/j.fertnstert.2011.11.036. PMID: 22192137; PMCID: PMC3277302.
- [8] Barber TM, Hanson P, Weickert MO, Franks S. Obesity and Polycystic Ovary Syndrome: Implications for Pathogenesis and Novel Management Strategies. Clin Med Insights Reprod Health. 2019 Sep 9;13:1179558119874042. doi: 10.1177/1179558119874042. PMID: 31523137; PMCID: PMC6734597.
- [9] Perelman D, Coghlan N, Lamendola C, Carter S, Abbasi F, McLaughlin T. Substituting poly- and mono-unsaturated fat for dietary carbohydrate reduces hyperinsulinemia in women with polycystic ovary syndrome. Gynecol Endocrinol. 2017 Apr;33(4):324-327. doi: 10.1080/09513590.2016.1259407. Epub 2016 Dec 2. PMID: 27910718.
- [10] Cunha NBD, Ribeiro CT, Silva CM, Rosa-E-Silva ACJS, De-Souza DA. Dietary intake, body composition and metabolic parameters in women with polycystic ovary syndrome. Clin Nutr. 2019 Oct;38(5):2342-2348. doi: 10.1016/j.clnu.2018.10.012. Epub 2018 Nov 3. PMID: 30449604.
- [11] Vuguin P, Sopher AB, Roumimper H, Chin V, Silfen M, McMahon DJ, Fennoy I, Oberfield SE. Alterations in Glucose Effectiveness and Insulin Dynamics: Polycystic Ovary Syndrome or Body Mass Index. Horm Res Paediatr. 2017;87(6):359-367. doi: 10.1159/000471804. Epub 2017 May 5. PMID: 28478437; PMCID: PMC5914159.