What is infertility?
To answer this question, first and foremost we need to establish what fertility means. Fertility is defined as the capacity to establish a clinical pregnancy; now the term infertility is somewhat harder to define since it’s used by some clinicians as a synonym for subfertility and sterility.
What are the differences between all these terms?
Using the definition of infertility as a focal point we can set confusion aside. Infertility is a disease characterized by the failure to establish a clinical pregnancy after 12 months of regular, unprotected sexual intercourse or due to an impairment of a person’s capacity to reproduce either as an individual or with his/her partner.
Subfertility is any form or grade of reduced fertility in couples unsuccessfully trying to conceive and sterility is a permanent state of infertility (1).
Infertility is common, with an estimate of 9 to 18% prevalence in general population, and according to the National Summary Report from the Society for Assisted Reproductive Technology, there were 190,394 cycles initiated in 2014 for egg retrieval, frozen embryo transfer and frozen egg thawing (2).
These numbers show that there are a lot of women going through some kind of infertility treatment. In this text we will take a deep dive into its correlation with obesity.
Which risk factors contribute to infertility?
- Ovulatory Disorders
One of the most common causes of female infertility. There are conditions such as polycystic ovary syndrome that affect the menstrual cycle in a way that disrupt the release of ovules, making them absent or irregular.
- Fallopian Tube Blockage
Previous infections such as pelvic inflammatory disease or cervicitis, surgeries and myomatosis cause changes in the fallopian tube anatomy and histology that can lead to a blockage, therefore making it difficult for the ovules to pass through them.
- Endometriosis
This is a common condition where uterine tissue grows outside the uterus, this causes abdominal or pelvic pain and inflammatory changes that impede the fertilization of the ovule. When endometriosis is classified as mild, female patient prospects for natural conception without treatment. Severe endometriosis demands treatment for infertility without delay (5).
- Uterine abnormalities
Congenital abnormalities, fibroids, myomatosis or polyps also causes infertility in females.
- Hormonal imbalances
Hyperprolactinemia usually causes amenorrhea but can be associated with normal ovulatory cycles, and its relevance to otherwise unexplained infertility is questionable. Hyperprolactinemia accounts for 10% to 15% of patients with amenorrhea but seldom causes only oligomenorrhea (1% to 2%) and, rarely, follicular dysfunction (luteal deficiency) in normally cycling females (5).
- Lifestyle and environmental factors
Regular sexual intercourse, two to three times per week beginning soon after menses, is an important determinant for the occurrence of pregnancy (1). It is well established that calorie restriction and excessive exercise causes a reduction in the frequency of ovulation in females.
- Stress and Emotional factors
Gaskin et al. demonstrated, in the female nurse population, that working longer hours (over 40 h/week) is associated with increased time to conceive, suggesting a relation of tiredness or stress with reduced fecundity (1).
Why and how is obesity correlated to infertility in females?
Obesity has become a major issue and a global epidemic, affecting more than 600 million adults worldwide. Females of reproductive age are no exception, and it is estimated that at least in the United States, 23% of them are now obese (3).
Obesity has a negative effect on reproductive potential, primarily thought to be due to functional alteration of the hypothalamic-pituitary-ovarian (HPO) axis, which is the one that causes production of gonadotropins (hormones that have a positive effect in fertility).
This happens because obese females have abnormal high levels of insulin in their blood, which makes their ovaries increase their androgen production (3). These androgens are converted into estrogens in the fat tissue, leading to tricking the body into blocking the HPO axis and clinically manifesting as menstrual abnormalities and ovulatory dysfunction in obese females.
Analysis of follicular fluid assayed for various hormones and metabolites from patients undergoing in vitro fertilization cycles demonstrates significant differences in obese female patients compared with their normal-body mass index (BMI) counterparts. Furthermore, the systemic alterations associated with obesity, namely, hyperinsulinaemia, dyslipidaemia and inflammatory responses, are evident from the ovarian follicular microenvironment (4).
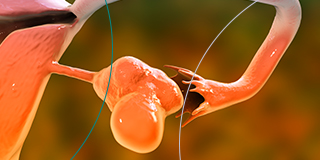
Effect of obesity on the oocyte
Obesity is a factor that also has a negative effect on oocytes. Oocytes are the female germ cells involved in reproduction, during the fetal period oocytes are produced, and they mature one by one each menstrual cycle during the extrauterine life of a female, converting into ovules. The oocyte yield is lower in obese females, and they have a higher rate of cycle cancellation (3).
Effect of obesity on the embryo
The preimplantation embryo is also affected by an obese environment. Comparison of human in vitro fecundation cycles with autologous oocytes show that obese females are more likely to create poor quality embryos (3). Among females undergoing in vitro fertilization, heightened concentrations of a particular omega-3 fatty acid known as alpha-linoleic acid were linked to reduced pregnancy rates.
Effect of obesity on the endometrium
There is a disparity in the research findings concerning whether obesity exerts a substantial impact on the endometrium. While certain studies investigating obese females who receive embryos from donor eggs have revealed no variance in implantation rates when compared to their non-obese counterparts, leading researchers to suggest that obesity does not impair endometrial receptivity. A retrospective analysis conducted by Desolle et al. involving 450 donor-oocyte frozen embryo transfer cycles demonstrated that BMI is an autonomous predictor of clinical pregnancy (3).
What are some potential interventions that could provide benefit to obese females seeking fertility?
- Weight loss
Kort et al. presented data from 52 overweight or obese females with infertility who were referred to weight loss counseling with a goal of 10% weight loss. A total of 32% of patients achieved the weight loss goal, and those patients had significantly higher conception rates (3).
- Physical Activity
There are studies that support regular physical activity independently from weight loss as a way to achieve higher pregnancy rates. In a retrospective cohort of obese infertile females undergoing 216 cycles of in vitro fertilization, the outcomes of patients that engaged in regular physical activity were compared with those who were sedentary, as assessed by the validated Global Physical Activity Questionnaire. There were significantly higher pregnancy rates in the active group (41 cycles), with a 3.71 relative risk of live birth (3).
- Dietary Factors
It is highly probable that fertility is influenced not only by an excess of calorie consumption but also by the way those calories are distributed among different food groups.
- Bariatric Surgery
According to the American Society for Metabolic and Bariatric Surgery (ASMBS), surgery can be the most effective treatment for people battling with severe obesity or other medical problems like heart and kidney disease (6).
Implications of Female Infertility
The emotional toll of infertility is substantial, impacting a woman’s mental well-being and self-esteem. The pressure to conceive can strain relationships and lead to feelings of inadequacy, depression, and anxiety.
Women often internalize their infertility struggles, creating a sense of isolation and sadness.
The financial burden of fertility treatments is also a concern. In vitro fertilization (IVF) and other assisted reproductive technologies can be costly, and insurance coverage varies widely. The financial strain adds an additional layer of stress to couples already dealing with infertility.
Conclusion
Infertility in women is a multifaceted issue with numerous potential causes, ranging from physiological factors to lifestyle and environmental influences. Understanding these causes is crucial for both healthcare professionals and individuals struggling with infertility.
It’s important to approach infertility with compassion and empathy, recognizing the emotional toll it takes on couples and the financial challenges they may face.
Seeking timely medical intervention and emotional support can help couples navigate the challenges of infertility and, in some cases, find solutions that enable them to achieve their dream of parenthood.
Research and awareness are essential in addressing this issue and ensuring that women facing infertility have the resources and support they need to cope with and overcome this challenging experience.
Contact Us Today
Our team is ready to help you. At LIMARP, patients will always receive warm, sincere and professional
answers. For a free evaluation please call us at (619) 270 8823, fill out a contact form at
our website, or message through any of our social media pages.
References
- Melodie Vander Borght, Christine Wyns. Fertility and infertility: Definition and epidemiology. ELSEVIER. Clinical Biochemistry 62 (2018) 2-10
- Brent Hanson, Erica Johnstone, Jessie Dorais, Bob Silver, C. Matthew Peterson, James Hotaling. Female infertility, infertility-associated diagnoses, and comorbidities: a review. Assisted Reproduction Technologies. (2016)
- Darcy E. Broughton, M.D. and Kelle H. Moley, M.D. Obesity and female infertility: potential mediators of obesity impact. American Society for Reproductive Medicine. (2017)
- Talmor A, Dunphy B. Female Obesity and Infertility. Best Practice and Research Clinical Obstetrics and Gynaecology (2014)
- Michael G. R. Hull, MD. David J. Cahill, MD. Female infertility. Gonadal Disorders. Volume 27-Number 4. December 1998.
- “Benefits of Weight Loss Surgery”. https://asmbs.org/patients/benefits-of-weight-loss-surgery. (Accessed on October 21, 2023).