Gastrointestinal leaks in Gastric Sleeve Surgery
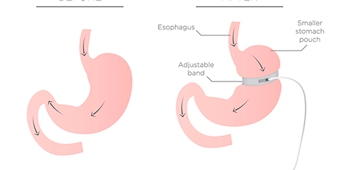
The gastric sleeve surgery, also known as the sleeve gastrectomy, is the most requested and practiced bariatric surgery worldwide [1]. Out of all the bariatric surgeries performed in 2019, 59% accounted for gastric sleeve surgeries, according to the latest IFSO report [1]. The gastric sleeve surgery is also one of the safest bariatric surgeries available, as it is the one with the most documented data about its short-term and long-term outcomes in research studies, and consequently it is the most standardized procedure in the field. However, every medical treatment and surgery comes with its own risks. In the case of gastric sleeve surgeries, its benefits highly outweigh its risks, as it helps to control, and even overcome, different comorbidities associated to obesity, such as type II diabetes, hypertension, heart diseases, infertility, and so much more.
The most serious risk about having any bariatric surgery is the development of a gastrointestinal leak. Common bariatric operations that can lead to leakage are the Roux-en-Y gastric bypass, the duodenal switch and, unfortunately, the gastric sleeve surgery [2]. A gastrointestinal leak is one of the most dreaded complications of bariatric surgery because it carries a significant mortality and morbidity risk [2], it is also difficult to diagnose because its symptoms may vary and because some radiological studies and test might give deceitful results [3].
Types of gastrointestinal leaks
A gastrointestinal anastomotic leak is “a leak of luminal contents from a surgical join between two hollow viscera”, according to a standard definition provided by the UK Surgical Infection Study Group [4]. A leak can be classified according to the time of their emergence as [4]:
- Early leak: which may appear between day 1 and 3 after surgery.
- Intermediate leak: which appears between day 4 and 7 after surgery.
- Late leak: it develops during or after day 8 of surgery.
They can also be classified according to their location or reason of development. Some leaks are due to technical difficulties during surgery, but others are due to patient-related factors such as poor nutrition, recent or current smoking history, liver cirrhosis, or renal failure [2]. Also, depending on their severity, a leak may be either subclinical or clinical [4]. All these aspects matter greatly because each type of leakage manifests its own set of symptoms and determines the appropriate action for its management.
How common is it?
Considering the fact that bariatric surgeries are very safe and most of the end up pretty successfully, the gastrointestinal leak is regarded as the most common complication for which surgeons have to be especially vigilant, although its incidence is fairly low.
The incidence of gastrointestinal leaks after a gastric sleeve surgery tends to vary in each research study, depending on their procedures and methodology. According to the International Sleeve Gastrectomy Expert Panel Consensus Statement of 2011, based on a data of 12,799 laparoscopic gastric sleeve surgeries, the leak rate was of 1.06% [5]. However, the leak rate reported on bariatric literature varies between 1 to 5% of patients that undergo gastric sleeve surgery [2,3,4] for a primary procedure and more than 10% for those receiving a revision procedure [5]. The higher leak risk in revision of previous bariatric surgery might be due to the increased dissection required by re-operative surgery [3].
Common symptoms
Physical symptoms of a gastrointestinal leak after gastric sleeve surgery include:
- Tachycardia (increased heart rate) higher than 120 beats per minute
- Fever higher than 37 ˚C or 98.6 ˚F
- Respiratory distress or tachypnea with more than 18 breaths per minute
- Worsening abdominal pain
- Chest pain and/or shoulder pain
- Dizziness
- A general feeling of illness and anxiety
Please consult your bariatric surgeon immediately if you experience any of these symptoms after your surgery. These symptoms tend to worsen in the next days and won’t get any better unless you get immediate medical attention. Your doctor will practice protocol screenings that will help to determine if you need further intervention. Don’t allow these symptoms to progress or evolve, notify them right away, as early diagnosis and management is fundamental for avoiding further complications.
Other clinical symptoms of a leak after gastric sleeve surgery include:
- Increased white blood cell count
- Increased C-reactive protein levels
Symptoms vary depending on the type of gastrointestinal leak. E.g., tachycardia is the earliest symptom in patients with an early leak, but fever is the earliest symptom in patients with intermediate and late leaks [4]. In some cases, patients with a gastrointestinal leak remain asymptomatic, which makes it even more difficult to diagnose. In these cases, the detection of the leak relies on the frequent monitoring of the patient with radiographic imaging. The leak usually manifest itself after the radiography screening. This is one of the many reasons why it is very important that every bariatric patient complies to their follow-up consultations and tests, even if you are feeling okay.
Symptoms of a gastrointestinal leak can vary from patient to patient and some might even fail to recognize them until they get worse. Because of this, a gastrointestinal leak after a gastric sleeve surgery can take an average of 3.9 to 2.6 days to be diagnosed and intervened [3]. Be extra vigilant of your body during the first weeks after your gastric sleeve surgery and talk to your surgeon as soon as possible if you start experiencing any of the symptoms described above. A day or two can make a difference in the management of a gastrointestinal leak after gastric sleeve surgery.
Interventions for a leak after gastric sleeve surgery
Not all leaks require operative management [3]. Some patients do require operative interventions, while others can overcome the leakage with non-operative treatments like percutaneous drainage techniques or prophylactic drains. This depends, of course, on the type and severity of the gastrointestinal leak. However, early detection of the leak is fundamental for its successful intervention and to avoid life threatening complications.
Surgeons should remain highly suspicious of any symptom like abdominal pain, fever, tachycardia and difficult breathing after gastric sleeve surgery, and should explore the patient thoroughly. To discard any suspicion of a leak after a gastric sleeve surgery, surgeons should take radiographic scans or exploratory laparoscopy and blood tests.
The management and intervention for a leak after a gastric sleeve surgery varies according to the clinical evaluation, the time of diagnosis and the location of the leak [5].
Complications caused by a gastrointestinal leak
Failure to detect and treat a gastrointestinal leak after gastric sleeve surgery in a timely manner can lead to [4]:
- Gastric ulcers
- Fistulas
- Peritonitis
- Septic shock
- Multisystem organ failure
- In the worst-case scenario, death
These complications can be avoided with an early diagnosis. A later diagnosis increases the risk and severity of possible complications. If you received gastric sleeve surgery and are experiencing tachycardia, fever, abdominal pain or difficult breathing, do not hesitate and notify your doctor as soon as possible.
Preventive measures to avoid a leak and further complications
Is there a way to prevent a leak after gastric sleeve surgery? Most of the preventive measures fall on the surgeon and its surgical team. We will get to that on further paragraphs; however, there are a few simple measures that every patient can take to avoid a leak after their gastric sleeve surgery:
- Truly rest after your surgery. During the first few weeks of your surgery you should focus on your recovery by providing your body the proper rest it needs. Do not carry heavy objects and avoid going up and down many stairs. Delegate any activities you might have or ask for help if there’s anything you need.
- Comply with every post-operative instruction. Take every medication that the surgeon prescribes and be mindful of any recommendation.
- Commit to your post-operative diet. Stick to liquids for the amount of time that your doctor prescribes. Eating solids way to soon could cause complications for your digestive system while it is still recovering.
- Notify your doctor of any symptoms, immediately. If you find yourself experiencing any fever, tachycardia, difficulty breathing, high anxiety, abdominal pain, nausea or vomiting during the first post-operative month, notify your doctor right away. Don’t wait for these symptoms to evolve. An early diagnosis and treatment can prevent any further serious complications.
- Attend every post-operative and follow-up consultation. Make sure you don’t skip or forget any follow-up consultation. Frequent monitoring is fundamental for the prevention of any risks and complications after gastric sleeve surgery, or any bariatric surgery, for that matter.
- Avoid nonsteroidal anti-inflammatory drugs. NSAIDs can cause ulcers and other complications after bariatric surgeries. Your doctor will prescribe proper pain medicine after your bariatric procedure. Stick to what your doctor tells you. If you want to take other medication, always ask your doctor first. Self-medication is very dangerous in this scenario (and in any other).
Your medical team will also take proper measures to prevent any leaks in their bariatric patients, such as:
- A careful patient selection. Not every patient is eligible for bariatric surgery. Gastric sleeve eligibility depends on many factors, such as the patient’s body mass index and any obesity associated comorbidities. Previous clinical history is also important. Choosing the correct patient for gastric sleeve surgery from the start can prevent complications like a gastrointestinal leak after surgery.
- An adequate surgical procedure. The technical experience of the surgeon is of paramount importance. Choosing the right surgeon from the start is the best preventive measure for most risks after bariatric surgery. You can trust your bariatric procedure to the expert hands of Dr Liza María Pompa González at LIMARP, Master Surgeon certified by the Surgical Review Corporation.
- Regular screenings. Every patient should comply with their post-op tests, screenings and appointments in order to identify any suspicious symptoms.
- Maintenance of high suspicion of any symptoms like tachycardia, fever or abdominal pain during the first weeks or months after the gastric sleeve surgery, and make exploratory screenings and test immediately.
Contact us for a consultation today
Dr. Liza María Pompa González and her bariatric team at LIMARP International Center of Excellence for Bariatric Surgery, located at Tijuana, Mexico, have performed thousands of gastric sleeve surgeries to patients who travel from all over the world. LIMARP offers an integral bariatric program that tackles obesity from a multidisciplinary approach, considering bariatric interventions along with psychological, nutritional and physical counselling. Our bariatric solutions include surgical interventions such as the gastric sleeve surgery, the gastric bypass, the mini gastric bypass, and the duodenal switch; and non-surgical solutions like the intragastric balloon. We also offer cosmetic solutions after bariatric surgery for those patients seeking further enhancements.
Our practice is an outstanding medical tourism clinic in Tijuana that offers all inclusive packages for patients traveling from abroad. We make travel easier for you, as we offer lodging in our luxurious next-door Grand Hotel Tijuana and transportation from the airport to the hotel and back. At LIMARP you get to experience quality service, convenience and comfort at a competitive price.
If you are interested in knowing if a gastric sleeve surgery is the right choice for you, give us a call to our phone number (619) 270-8823 or send us a message through this webpage or any of our social media accounts. Contact us today to schedule your initial consultation. Our team of experts will take you through all your options for obesity treatment and will offer a personalized plan tailored to your specific needs.
Bibliography
- [1] International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) (2019). Fifth IFSO Global Registry Report 2019. https://www.ifso.com/pdf/5th-ifso-global-registry-report-september-2019.pdf
- [2] Nguyen, N. T.; Daly, S. C. (2020). Management of Gastrointestinal Leaks and Fistula. In Ninh T. Nguyen, Stacy A. Brethauer, John M. Morton, Jaime Ponce & Raul J. Rosenthal (eds.), The ASMBS Textbook of Bariatric Surgery (2nd ed.). Springer.
- [3] Bekheit, M.; Katri, K. M.; Nabil, W.; Sharaan, M. A.; El Kayal, E.S. A. (2013). Earliest signs and management of leakage after bariatric surgeries: Single institute experience. Alexandria Journal of Medicine, 49: 29-33. https://www.sciencedirect.com/science/article/pii/S2090506812000899
- [4] Burgos, A. M.; Braghetto, I.; Csendes, A.; Maluenda, F.; Korn, O.; Yarmuch, J.; Gutierrez, L. (2009). Gastric Leak After Laparoscopic-Sleeve Gastrectomy for Obesity. Obesity Surgery, 19: 1672-1677. https://pubmed.ncbi.nlm.nih.gov/19506979/
- [5] Abou Rached, A.; Basile, M.; El Masri, H. (2014). Gastric leaks post sleeve gastrectomy: Review of its prevention and management. World Journal of Gastroenterology, 20 (38): 13904-13910. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4194572/