Gastric bypass surgery is one of the most common bariatric procedures available for patients who are dealing with morbid obesity, hypertension, and type 2 diabetes. This surgery has proven to be useful for losing weight and for correcting or reducing other comorbid issues, such as hyperlipidemia, GERD, and lower back pain. The postoperative recovery process takes several months and if the procedure goes over smoothly, the patient should expect positive results, as long as they also follow their doctor’s recommendations on how to take care of their body.
These recommendations can include a determined resting period, prescribed medication, a specific diet, and removing certain habits from your daily life that could hinder your recovery. However, it’s important to keep in mind that all surgeries can have potential complications during and after the procedure, and the gastric bypass is not exempt from this. Some complications that may arise include infection, hemorrhages, hernias, and ulceration.
Our team at LIMARP®, led by Dr. Liza María Pompa González, takes care of you on each step of the surgical process so that any arising complication can be treated effectively and safely. We also like to keep our patients well-informed and the present article mainly focuses on the ulceration that may happen after the gastric bypass surgery, what causes it, and how to treat it.
Gastric Bypass: What Is It?
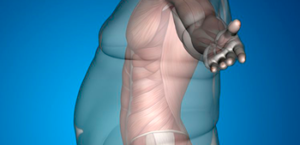
Gastric bypass surgery, also known as Roux-en-Y, is a technique that can be divided into two steps. The first one consists in making the stomach smaller by dividing into two sections with surgical staples; the top, smaller section is called a pouch and it’s where the food will go. The pouch only holds a certain amount of food, which will allow you to eat less. The second step is the bypass where your surgeon will connect part of your small intestine to the pouch so that the food that you eat goes directly from one to another. This means that your body will absorb less calories.
There are several variations to the gastric bypass and while their ultimate goal is the same, the techniques surgeons use to carry them out is what makes them different. Here are some of the types of gastric bypass:
- Roux-en-Y (proximal)
- Roux-en-Y (distal)
- Mini-gastric bypass
- Endoscopic duodenal-jejunal bypass
If you’re an eligible patient for gastric bypass surgery, your doctor will review your medical history and after an initial screening, they will determine which procedure is best for you and your needs.
An important part of the preoperative process is letting you know the risks and complications that may occur during and after the surgery, as well as the steps you can take to lower their chances. Prior to the procedure, your doctor may ask you to decrease your BMI, take up physical activity, and to stop smoking.
However, there’s a slight percentage that you’ll still experience some type of complication, regardless of the steps you took to prevent them. One of the most common ones is the anastomotic or marginal ulcer, which can occur in 1% to 16% of the patients.
What’s an Anastomotic Ulcer?
To get a clear idea of what an anastomotic ulcer is, let’s take a look at the term anastomosis. An anastomosis is a connection between two things that can branch out and in medical terms, it occurs when parts of the intestine or any other structure are connected through surgery, as is the case for the gastric bypass. An ulcer is a sore that appears on the body because the tissue was ruptured or abraded, or it can be a result of an infection.
An anastomotic ulcer, also known as marginal ulcer, is a common complication after gastric bypass surgery and it usually appears around the staple line, near the pouch, in cases where the distal stomach was stapled and not divided. This type of ulcer has higher risks of developing a month or two after the surgery, but it can also appear up to a year later. A marginal ulcer can cause nausea, vomiting, and abdominal pain for the patient, and in the worst of cases it can result in acute perforation or severe bleeding. These last two symptoms can occur because of a high production of gastric acid, which is a result of an enlarged pouch.
If you’re recovering from gastric bypass surgery and start experiencing any of the aforementioned symptoms, contact your doctor so that they can carry out an endoscopic evaluation and confirm the presence of the ulcer.
What Causes Ulcers?
There are many factors that can cause the formation of an anastomotic ulcer after the surgery, the most serious ones being smoking and the use of non-steroidal anti-inflammatory drugs (NSAIDS), which include over the counter aspirin, ibuprofen, and naproxen. The appearance of a partial anastomotic stricture can also lead to ulceration, as well as alcohol use and the presence of bacteria H. pylori. Another cause may be the presence of foreign bodies, such as the surgical staples along the pouch, because they “can lead to mucosal breakdown and ulceration”.
Your doctor can help you determine the underlying cause for the ulcer that developed during your postoperative process and establish a treatment to heal the damaged tissue. In most cases, the ulcer can be treated with medication such as proton pump inhibitors, cytoprotectants, and acid buffering agents; it’s only in extreme conditions where surgical intervention may be needed, such as extreme internal bleeding or for the removal of foreign bodies that are preventing the ulcer to heal.
Ulcer Prevention: Is It Possible?
There are several preoperative cautionary steps that you can take to prevent an ulcer from developing after gastric bypass surgery, such as a routine upper endoscopy to ensure that there is no bacteria in the area prior to the operation. If the patient is positive for H. pylori, they will be treated beforehand so that they can be as healthy as possible before going under the knife. Your surgeon may also recommend that you stop smoking and taking NSAIDS or any type of long-term anticoagulation. However, if you’re dependent on any type of medication that puts you at risk during the gastric bypass, your doctor may offer a different type of bariatric surgery to avoid an anastomotic ulcer or any other type of complications.
Another prevention measure can be carried out by your surgeon when performing the gastric bypass. A 2010 study suggested that “avoiding absorbable suture” can “reduce marginal ulcer development” and that proper surgical technique is critical. This is also something you can discuss with your doctor prior to your surgery to decide if this procedure is right for you.
Keep in mind that the experience of each patient can vary and not everyone will develop an ulcer during their recovery process. Our team of surgeons at LIMARP® are highly qualified and updated to ensure your safety during any bariatric procedure; they also oversee your healing process to prevent any complication from becoming unmanageable.
Contact Us to Learn More
If you’re recovering from gastric bypass surgery and experiencing any of the aforementioned symptoms, schedule an appointment with one of our doctors to check for an ulcer. We can help determine the right treatment for you. Contact us online anytime or give us a call at (619) 373-0229.